Sundowning: Late-Day Confusion in People with Dementia
People with dementia or cognitive impairment may become confused, irritable, or even aggressive at the end of the day. Learn how to help.

If someone you care about has cognitive impairment or dementia, you might notice them acting differently in the late afternoon or early evening. Sundowning, also known as sundowners or sundown syndrome, refers to a group of behaviors, feelings, and thoughts that people with cognitive impairment or dementia can experience in the late afternoon or evening, as the sun sets (but it can occur at other times as well). It can affect a person’s memory, thinking, personality, reasoning, and mood.
People experiencing sundowning may feel sad, anxious, fearful, restless, and irritable. In some cases, it can cause paranoia, delusions, and hallucinations. Typical behaviors include:
- Confusion
- Pacing, wandering, or rocking in a chair
- Shadowing (when the individual closely follows their caregiver everywhere they go)
- Crying
- Insomnia
- Ignoring directions
- Aggression, yelling, and in some cases even violence
Causes of sundowning
While not specific to any one disease or condition, sundowning is common in people experiencing dementia due to Alzheimer’s disease. One in five people living with Alzheimer’s experiences it at some point. It can also occur in the context of other illnesses that cause dementia and impair cognitive abilities, such as vascular dementia, diffuse Lewy body disease, and fronto-temporal dementia. Some medical conditions, such as kidney or liver dysfunction, thyroid disease, and others, may also be accompanied by sundowning.
The role of cognitive reserve
While the exact cause of sundowning remains uncertain, cognitive reserve may play a pivotal role in its underlying mechanisms. Cognitive reserve pertains to the brain's capacity to cope with neural changes, often influenced by educational and life experiences. Enhanced cognitive reserve, built over time, can serve as a protective factor against dementia. The interplay of diminished sensory input during sunset and increased cognitive demands in unfamiliar settings, coupled with compromised cognitive reserve due to underlying conditions, may lead to confusion, delirium, and sundowning symptoms.
Factors that may aggravate sundowning include:
- Unfamiliar surroundings
- Low lighting or increased shadows
- Fatigue or boredom
- Pain
- Depression
- Hunger or thirst
- Disruptions of the body’s internal clock
- Difficulty separating reality from dreams
- Presence of an infection, such as a urinary tract infection
Medication for sundowning
Treating the underlying trigger is the most effective way to resolve sundowning, but there are other options. The individual behaviors, feelings, and thoughts of people who go through sundowning can sometimes be treated with medications, including:
- Antidepressants and/or anxiolytics can help by treating underlying symptoms.
- Antipsychotics are commonly prescribed, but evidence is mixed (most studies do not directly target sundowning, focusing instead on delusions, hallucinations, and agitation).
- Melatonin may help, but current research is not conclusive.
- Cholinesterase inhibitors have been shown to decrease the behavioral disturbances in patients experiencing sundown syndrome.
Non-Medication Treatments
Light therapy has shown positive results in small studies, but larger controlled trials have not been conducted. Besides the lack of robust supporting evidence, ensuring a gradual transition from daylight to artificial light may ease behavioral changes occurring in the late afternoon and is commonly suggested by health care providers.
Environmental changes, music therapy, aromatherapy, and caregiver education can also help.
What you can do
If you are the caregiver for someone experiencing sundowning, there are many things you can do to help:
- Natural light can help reset the body’s internal clock and can also positively influence mood. It’s best to go outside if possible, but even sitting by a window can help. Avoid blue light (from devices such as cell phones and TVs) in the evenings and make sure there is darkness or low light at bedtime. If the person is agitated in the dark or in unfamiliar surroundings, you may turn on a night light.
- Physical exercise is critical and can enhance physical, mental, and emotional well-being, and improve sleep, all of which can help prevent sundowning.
- Keep to regular times for waking and going to sleep. Limiting daytime napping will encourage nighttime sleepiness.
- Limit sugar, alcohol, and caffeine in the evening to help the brain power down.
- Stick to a stable, predictable schedule that has meaning for the person. Keeping to regular times for waking up and going to bed, meals, and activities helps regulate the body’s internal clock and decrease stress and anxiety.
- Avoid excessive stimulation (auditory or visual) in the evening. Minimize unnecessary noise from visitors, loudspeakers, clattering dishes, loud conversations, or anything else you can control. Play familiar, gentle music or relaxing nature sounds, such as the sound of waves.
- In strange or unfamiliar settings, bring familiar items such as family photographs to help create a more relaxed and reassuring environment.
- If the person wears eyeglasses or hearing aids, make sure they are available and working correctly.
If problems persist
If sundowning continues to be a problem, seek medical advice. A medical exam may identify a specific trigger, such as pain, a sleep disorder or other illness, or a medication side effect. In addition, medical evaluation will help diagnose underlying conditions that, if treated, can reduce the risk of further episodes.
If medication is prescribed to help your loved one relax, control agitation, or sleep better at night, be sure to find out about possible side effects. Some medications can increase the chances of confusion, dizziness, and falls. Using such medications is only recommended for short periods of time and under close medical supervision.
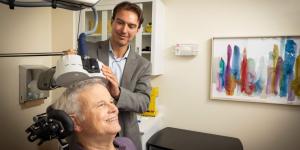
Dementia caregiver support in Boston
The Family Caregiver Program at the Deanna and Sidney Wolk Center for Memory Health provides support to family caregivers and their loved ones with dementia. We can assess your needs, provide you with skills and support to navigate caregiving, and tailor resources. Our services for caregivers and loved ones include skill-building and support groups and the opportunity to meet one-on-one with a family caregiver specialist for individual therapy. We are committed to providing culturally responsive care and our recommendations are based on your needs, including your social, spiritual, and financial situation.
If you or someone you know is struggling with the daily tasks of being a family caregiver to a loved one with dementia, we are here (and happy) to help offer support. Contact us today.
Blog Topics
Learn More
Free Guide to Brain Health
Download our free guide, “Optimizing Your Brain Health,” for expert advice on boosting brain health at any age. Explore practical tips and resources from Hebrew SeniorLife’s Deanna and Sidney Wolk Center for Memory Health.

Coping with Memory Loss
From our Wolk Center for Memory Health to Assisted Living to Memory Care Assisted Living, we offer a wide range of memory care services and support.
Long-Term Chronic Care
Hebrew Rehabilitation Center provides person-centered extended medical care in a homelike setting for patients with chronic illness. As a licensed long-term chronic care hospital, we provide higher-level, more comprehensive medical care to older adults than a traditional nursing home.