Non-Invasive Brain Stimulation Shows Promise for People with Parkinson’s Disease
Discover the ways researchers are exploring non-invasive brain stimulation to manage Parkinson’s disease gait changes.

With an average age of diagnosis of 60, Parkinson’s disease is often diagnosed later in life. It is a progressive neurodegenerative disorder that damages brain cells that produce dopamine, the chemical that helps coordinate movement. As dopamine levels drop, Parkinson’s can cause symptoms including shaking, stiffness, tremors, freezing of gait, and difficulty walking. When that happens, everyday tasks become more challenging.
Freezing of gait, defined as the “temporary, involuntarily inability to move,” is a dangerous and unpredictable symptom that many people with Parkinson’s disease experience. When someone experiences freezing of gait, they may lose balance, leading to falls that are particularly dangerous for older adults. Freezing of gait and other gait changes become even more likely as the disease progresses, making mobility unpredictable.
As an assistant scientist at Hebrew SeniorLife’s Hinda and Arthur Marcus Institute for Aging Research, I am interested in exploring effective, non-invasive treatment methods for Parkinson’s gait changes. One promising area of study is non-invasive brain stimulation, including transcranial direct current stimulation and transcranial temporal interference stimulation. These techniques offer hope for improving gait and enhancing the quality of life for those with Parkinson’s disease.
Transcranial direct current stimulation and gait
A commonly used treatment for Parkinson’s disease is deep brain stimulation, which involves implanting an electrode into the brain. Deep brain stimulation primarily targets tremors and is effective for some patients, but typically offers only limited relief for symptoms that disrupt the ability to walk. As an inpatient surgery, deep brain stimulation is also invasive and has a lengthy recovery time.
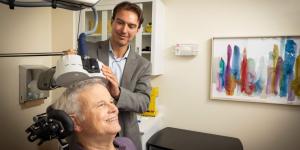
“There is a desperate clinical need for safe, noninvasive therapies to help patients suffering from Parkinson’s disease walk more safely throughout the day,” says Brad Manor, PhD, director of the Mobility and Falls Program at the Marcus Institute. He decided to study whether transcranial direct current stimulation, or tDCS, could be an effective treatment for freezing of gait.
Transcranial direct current stimulation works by sending low-level electrical currents between small electrodes placed on the scalp. This nonpainful process creates an electric field over the brain’s surface that influences how nerve cells — also known as neurons — function. More specifically, it alters how easily neurons can activate.
Specific parts of the brain need to be activated to experience the world around us and respond accordingly — for example, feeling the ground beneath our feet, making decisions, and especially when completing complex tasks like walking down a busy hallway. Dr. Manor’s research explored whether tDCS could make neurons more excitable and responsive, potentially improving gait and mobility for those with Parkinson’s disease.
“We aimed to increase the excitability of two different brain regions, one involved in coordinating muscle contractions and another that is very closely involved with cognitive functions like paying attention and making decisions. Interestingly, each of these regions is close to the surface of the brain and can be reached by tDCS, yet each has direct connections to the basal ganglia deep in the brain. The hope is that by increasing the ability to activate these brain regions, we can make it easier for patients with Parkinson’s disease to initiate and maintain a safe walking pattern, even while navigating complicated and ever-changing environments,” explains Dr. Manor.
The study found that tDCS showed promising results, especially for people with mild to moderate freezing of gait symptoms. The effects were not as clear across all participants, meaning it does not appear to be as effective when freezing of gait becomes severe in more advanced stages of the disease. “tDCS offers a safe option for some patients that is much safer than deep brain stimulation and maybe more specific to ‘freezing’ and other symptoms that disrupt walking,” explains Dr. Manor.
Transcranial temporal interference stimulation: The next frontier
Deep brain stimulation has been used for years for Parkinson’s but is less effective for gait and is a significant undertaking for patients. tDCS shows promise for gait but can only stimulate the brain superficially and may not be effective for those with more severe freezing of gait. There is now a way to use non-invasive technology to stimulate deeper parts of the brain and target gait-related symptoms like freezing: transcranial temporal interference stimulation, or tTIS.
tTIS delivers a set of high-frequency currents that can pass through the scalp and brain tissue and reach deep brain regions. Then, a low-frequency interference current is generated at the targeted deep brain region, which can change how the neurons in that region behave. That can help treat conditions like Parkinson’s, where damaged neurons in deep brain regions cause symptoms.
Our pilot study measured motor symptoms before, immediately after, and up to 60 minutes after receiving tTIS treatment. We found a significant reduction in motor symptom severity, with effects lasting up to an hour. These results show the potential of tTIS for improving motor function and movement for those with Parkinson’s. In other words, it provides a middle ground between tDCS and deep brain stimulation, offering deeper stimulation without invasive surgery.
Home-based brain stimulation is more accessible
It can be difficult for people with mobility limitations to travel for clinical trials and participate in in-person interventions. However, that doesn’t mean they should be excluded from research opportunities!
Knowing this, much of our focus has shifted to making our research more accessible. For example, a smartphone-based gait assessment I developed with Dr. Manor offers a specific type of gait analysis typically done in laboratory settings. In another blog post, Dr. Manor unpacks the importance of the smartphone-based gait assessment and other smart technology reshaping how freezing of gait is measured.
Remote technology has also extended to brain stimulation. Over the past several years, we have worked to create a home-based brain stimulation program where we can train family members and caregivers on how to safely deliver the stimulation while we monitor remotely. We will continue to prioritize these remote efforts, knowing that they make our clinical trials and treatment advances more accessible to the people who need them most.
The future of brain stimulation research
Transcranial direct current stimulation and transcranial temporal interference stimulation are emerging as exciting and non-invasive treatment options for freezing of gait in Parkinson’s disease. Compared to deep brain stimulation, these approaches appear to more specifically target walking-related symptoms, making them more precise and less invasive options for those experiencing mobility challenges.
Continued research and funding will help advance these treatments as we learn even more about how they could benefit those with Parkinson’s.
Get personalized fall prevention strategies for your home
If you or a loved one is experiencing movement symptoms related to Parkinson’s disease, Hebrew SeniorLife’s Home Health team may be able to offer valuable support.
Getting to the doctor’s office to get support and ask questions can be tough. With a referral from a doctor, our Home Health professionals can evaluate your risk for falls and recommend home modifications to enhance safety and independence. Learn more about our Home Health services today.
Join Our Community: Subscribe to the Hebrew SeniorLife blog for weekly insights on healthy aging and senior living.
Blog Topics
Learn More
Home Health
Hebrew SeniorLife Home Health will send registered nurses and home health aides to your home to provide skilled care any time you need it.
Research on Aging
At the Hinda and Arthur Marcus Institute for Aging Research, Harvard Medical School-affiliated researchers are working to uncover answers to some of the most pressing challenges of aging.